The symptoms of endometriosis
1 in 10 people with a cervix of reproductive age has endometriosis1. As a healthcare professional in the UK, this means you’re likely to see patients with the condition every day.
Perhaps their symptoms don’t scream endometriosis. Perhaps they sound more like a urinary tract infection (UTI), irritable bowel syndrome (IBS) or pelvic inflammatory disease (PID)2,3. It’s this overlap that can cause delays3.
But you have the power to help end the eight-year wait4 for a diagnosis. Just listen out for these endometriosis symptoms in your consultations... and start raising the red flag:
Pelvic pain
This is often at its worst around the time of a patient’s period. And endometriosis pain can be so debilitating it interrupts their daily life3,5-7.
Heavy periods
Your patient’s periods are so heavy their tampons or pads need changing constantly. They might also talk about leaking and blood clots3,5-7.
Painful sex
Dyspareunia – pain just before, during or after sex – is a common symptom of endometriosis3,5-7.
Gastro/urinary problems
Constipation, diarrhoea and pain when urinating or emptying their bowels are all red flags3,5-7. Your patient might also see blood in their urine or stools3,5-7.
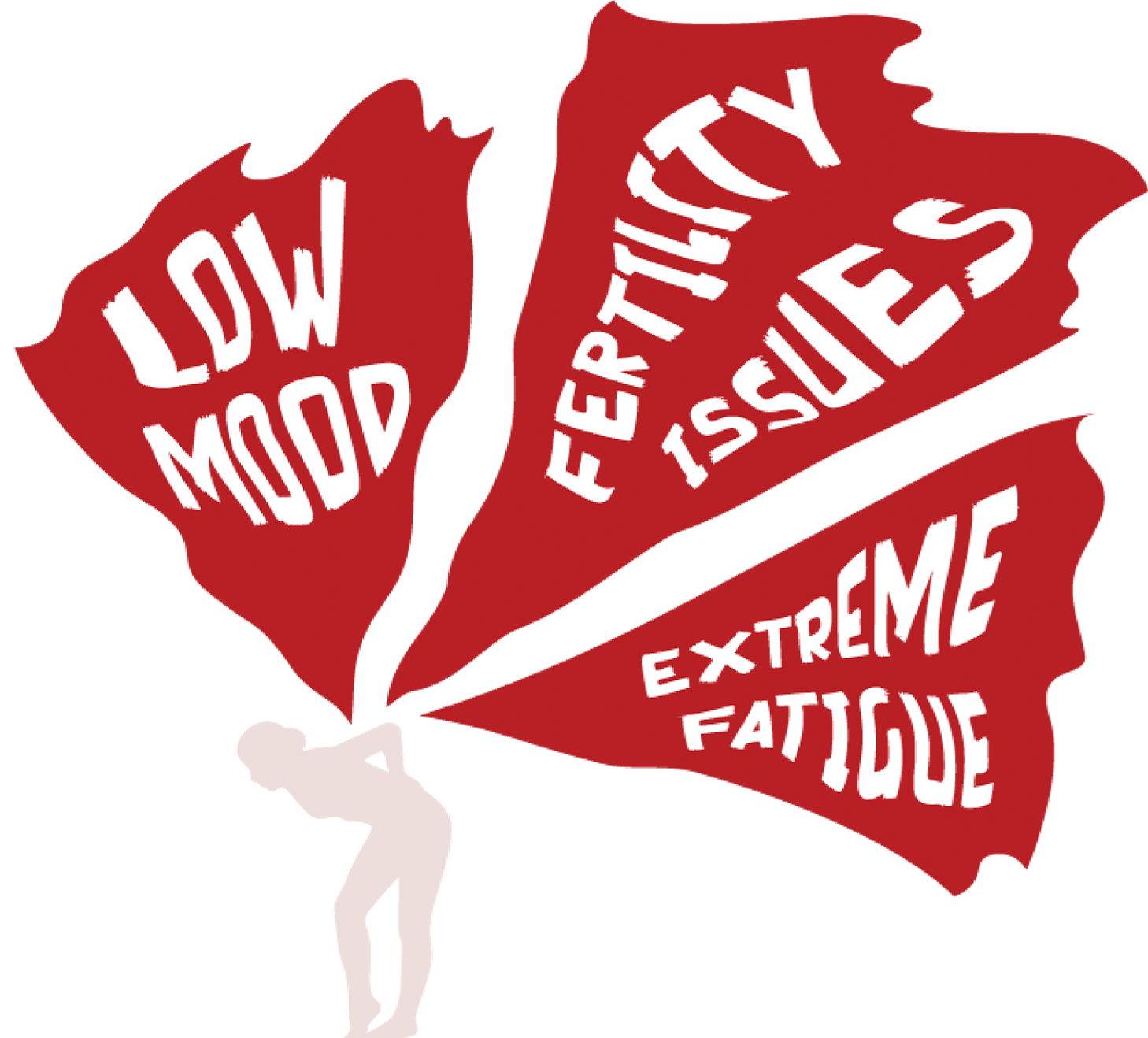
Low energy, low mood
Over half of patients with endometriosis feel down, depressed or hopeless5. Exhaustion is common too. Almost a third of people with the condition feel tired and weak5.
Fertility issues
If your patient is having trouble conceiving 3,5-7 and they have one or more of the symptoms above, it’s time to raise the red flag.
What's causing your patients' symptoms?
Endometriosis pain, heavy periods, and the other debilitating symptoms of endometriosis occur because cells – similar to those in the endometrium – grow outside the uterus. They can envelop the ovaries and the fallopian tubes. They can also grow on nearby organs like the bowel and bladder2,7.
Endometriosis symptoms are often worse around the time of a patient’s period because, every month, these cells build up, break down and then bleed. With no way for this blood to leave the body, the pelvic area can become inflamed and painful scar tissue can grow2,7.
These symptoms can start as soon as a young patient begins their period and, they can last until menopause7.
References:
- Rogers PA, D'Hooghe TM, Fazleabas A, et al. Priorities for endometriosis research: recommendations from an international consensus workshop. Reprod Sci 2009;16(4):335-46.
- Horne AW, Missmer SA. Pathophysiology, diagnosis, and management of endometriosis. BMJ. 2022;379:e07075
- National Institute for Health and Care Excellence. 2017. Endometriosis: Diagnosis and Management. [NICE Guideline No.73]. Available from: https://www.nice.org.uk/guidance/ng73. [Accessed Feb 2024].
- All Party Parliamentary Group on Endometriosis (APPG). Endometriosis in the UK: time for change. APPG on Endometriosis Inquiry Report 2020. Available from: https://www.endometriosis-uk.org/sites/default/files/files/Endometriosis%20APPG%20Report%20Oct%202020.pdf. [Accessed Feb 2024].
- Becker K et al. Real world data on symptomology and diagnostic approaches of 27,840 women living with endometriosis. Sci Rep. 2021 Oct 14;11(1):20404.
- NHS Endometriosis. Available from: https://www.nhs.uk/conditions/endometriosis/. [Accessed Feb 2024].
- World Health Organization (WHO). Endometriosis Fact Sheet. Available from: https://www.who.int/news-room/fact-sheets/detail/endometriosis. [Accessed Feb 2024].